ICD 10 CM Updates for 2025 Chapters 6 -11
Welcome to Part Two of an in depth review of this year’s new ICD 10 CM diagnoses codes. Coders and CDI specialists rely on provider documentation to assign codes. More often than not third party denials and appeals rely on clinical evidence to support the assigned diagnosis. This article provides both the coding and clinical evidence to support the new ICD 10 CM codes.
Chapter 6 Diseases of the Nervous System
KCNQ2 is not the name of a medical condition, however it is the name of the gene that is mutated in the 5 new KCNQ2 epilepsy codes in chapter 6. When epilepsy is traced back to a disease-causing (pathogenic) variant in the KCNQ2 gene, it is labelled a KCNQ2-related disorder. This is a type of epilepsy that is diagnosed in infants and children.
According to the Children’s Hospital of Philadelphia “Mutations in the KCNQ2 gene cause a range of neonatal-onset epilepsy syndromes, including severe early-onset epilepsies (developmental and epileptic encephalopathies) and milder presentations that are typically referred to as self-limited (benign) neonatal epilepsies, which may run in families. The symptoms a child experiences and the severity of the disorder can vary widely and will depend on the particular KCNQ2-related epilepsy the child has.”
“KCNQ2-related epilepsies fall into two broad categories as follows:
KCNQ2-developmental and epileptic encephalopathy (DEE)
Self-limited neonatal epilepsy
Seizures beginning shortly after birth may be the first indication of a KCNQ2-related epilepsy. However, the associated symptoms and outcomes can vary widely, depending on the particular KCNQ2-related epilepsy the child has.”
“KCNQ2-Developmental and Epileptic Encephalopathy
Encephalopathy refers to a disease that affects the functioning of the brain. Children with KCNQ2-developmental and epileptic encephalopathy typically experience multiple daily seizures that begin within the first week of life. These seizures are often tonic (stiffening) seizures and may be associated with jerking movements and changes in breathing or heart rate. Seizures are often associated with characteristic patterns on EEG and may be difficult to control with anti-seizure medications initially. Children with KCNQ2-developmental and epileptic encephalopathy have delays in reaching developmental milestones and associated cognitive impairment, ranging in severity from moderate to severe.”
KCNQ2-Related Epilepsies | Children's Hospital of Philadelphia
G40.84 KCNQ2-related epilepsy
G40.841 KCNQ2-related epilepsy, not intractable, with status epilepticus CC
G40.842 KCNQ2-related epilepsy, not intractable, without status epilepticus CC
G40.843 KCNQ2-related epilepsy, intractable, with status epilepticus CC
G40.844 KCNQ2-related epilepsy, intractable, without status epilepticus CC
Serotonin is a chemical produced by nerve cells and used to send signals between them. It is classified as a hormone and a neurotransmitter. Theories have suggested serotonin is associated with mood and mental wellbeing. Medications for mental health disorders change how the brain uses serotonin. Too much serotonin can be caused by taking a medication that boosts serotonin levels, with an increase in the dosage of an existing prescription, or use of an additional drug that also increases serotonin levels.
There was previously no code for Serotonin syndrome in ICD 10 CM and the coordination and maintenance committee added it due to the increased use of serotonergic agents prescribed to treat depression. The addition of the code allows for more accurate capture of the condition and the significant morbidity associated with it.
Serotonin syndrome is a potentially life-threatening condition associated with increased serotonergic activity in the central nervous system (CNS). Serotonin is associated with the regulation of appetite, sleep, memory, attention, thermoregulation, mood and sexual activity. Peripherally, serotonin modulates coagulation and smooth muscle contraction.2,3,4
G90.81 Serotonin syndrome CC
Notes:
Code first poisoning due to drug or toxin, such as:
linezolid (T36.8X- with sixth character 1-4) (T36.8X1A-T36.8X4S)
monoamine oxidase inhibitors (T43.1X with sixth character 1-4) (T43.1X1A- T43.1X4S)
selective serotonin and norepinephrine reuptake inhibitors [SSNRI] (T43.21 with sixth character 1-4) (T43.211A-T43.214S)
selective serotonin reuptake inhibitors [SSRI] (T43.22 with sixth character 1-4) (T43.221A-T43.224S)
Use additional code for adverse effect, if applicable, to identify drug, such as:
linezolid (T36.8X5) (T36.8X5A-T36.8X5S)
monoamine oxidase inhibitors (T43.1X5) (T43.1X5A-T43.1X5S)
selective serotonin and norepinephrine reuptake inhibitors [SSNRI] (T43.215) (T43.215A-T43.215S)
selective serotonin reuptake inhibitors [SSRI] (T43.225) (T43.225A-T43.225S)
Use additional code, if applicable, to identify:
disseminated intravascular coagulation (D65) (D65)
hypertensive crisis (I16.-) (I16-I16.9)
metabolic acidosis (E87.2-) (E87.2-E87.29)
shock, not elsewhere classified (R57.-) (R57-R57.9)
toxic encephalopathy (G92.-) (G92-G92.9)
ventricular tachycardia (I47.2-) (I47.2-I47.29)
G90.89 Other disorders of autonomic nervous system
G93.45 Developmental and epileptic encephalopathy CC
(Inpatient Only) HIV - HIV Related Dx
Chapter 7 Diseases of the Eye and Adnexa
Chapter 8 Diseases of the Ear and Mastoid Processes
There were no changes for Chapters 7 and 8 this year.
Chapter 9 Diseases of the Circulatory System
A “Fat Embolism” occurs when one or more droplet-like particles of fat enter the bloodstream and embolize to the systemic or pulmonary circulation. This is usually secondary to traumatic fractures.
A cement embolism is always a complication and should be treated as such. This results from cement used in Orthopedic procedures such as joint arthroplasty or spinal kyphoplasty escaping into the systemic circulation embolizing blood vessels in the peripheral or pulmonary circulation.
Cor pulmonale is defined as an alteration in the structure (e.g., hypertrophy or dilatation) and function of the right ventricle (RV) of the heart caused by a primary disorder of the respiratory system resulting in pulmonary hypertension. In the case of pulmonary emboli, regardless of the source, the increased resistance created from altered blood flow through the pulmonary vasculature causes increased work for the right heart. Massive pulmonary embolism is the most common cause of acute cor pulmonale. A massive pulmonary embolism can mimic a myocardial infarction with elevated troponins, ST changes, chest pain, and shortness of breath. According to NIH Right-sided heart failure secondary to left-sided heart failure, or congenital heart disease is not considered cor pulmonale. (Cor Pulmonale - StatPearls - NCBI Bookshelf)
I26.03 Cement embolism of pulmonary artery with acute cor pulmonale
Notes
Unacceptable Principal Dx (Inpatient Only)
MCC - Major Complication (Inpatient Only)
I26.04 Fat embolism of pulmonary artery with acute cor pulmonale
MCC (Inpatient Only)
I26.95 Cement embolism of pulmonary artery without acute cor pulmonale
Unacceptable Principal Dx (Inpatient Only)
MCC - Major Complication (Inpatient Only)
I26.96 Fat embolism of pulmonary artery without acute cor pulmonale
MCC - Major Complication (Inpatient Only)
Chapter 10 Diseases of the Respiratory System
Ten new codes were added to capture nasal valve collapse. According to the September 2023 Coordination and Maintenance Committee Nasal Airway Obstruction (NAO) is a source of significant patient discomfort. The anatomical cause of Nasal Valve Collapse (NVC) was described in the presentation as: “Weak or excessively flexible upper/lower cartilage in the outer nasal wall may cause it to collapse inward when a person inhales.”
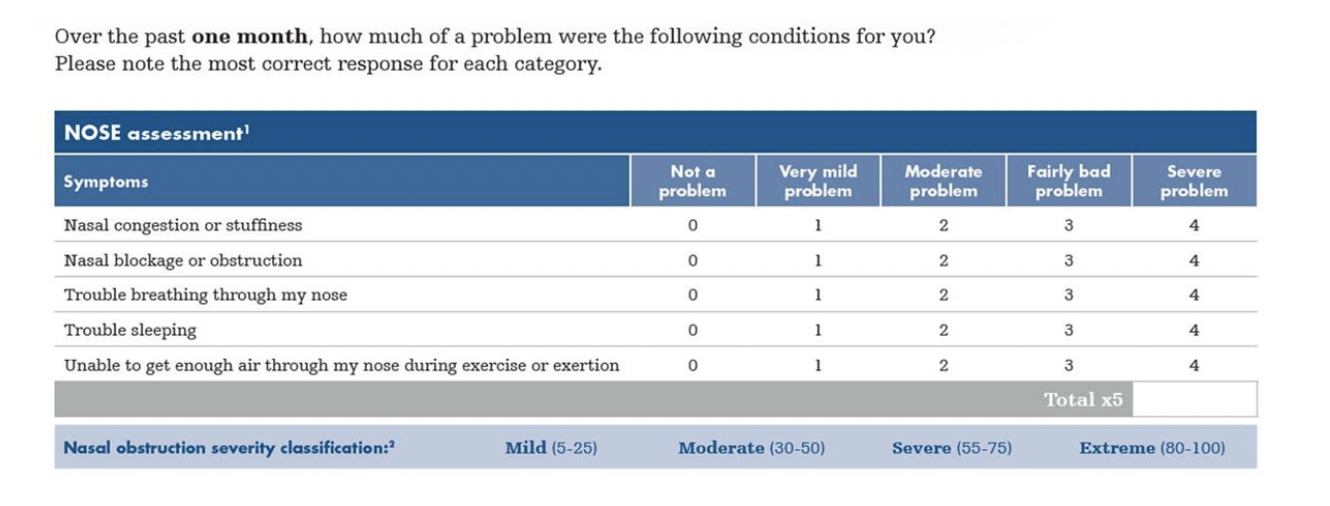
The American Academy of Otolaryngology (AAO), “NVC is a distinct clinical entity separate from other anatomical reasons for NAO.” The NOSE Score was identified as a valid standard of measure for severity.
The American Academy of Otolaryngology-Head and Neck Surgery really did the best job of explaining NVC when they provided this overview of Nasal Valve dysfunction:
“Nasal valve dysfunction is a common clinical cause of symptomatic nasal airway obstruction due to either narrowing or collapse of the nasal valve.1 The nasal valve consists of external and internal components. The external nasal valve is defined as the area bounded by the caudal septum, medial crus of the lower lateral cartilage, alar cartilage and fibrofatty tissue, and the nasal sill. The internal nasal valve is bounded by the septum, head of the inferior turbinate, and the upper lateral cartilage. Etiologies of external and internal nasal valve dysfunction can be further broken down into static and dynamic causes. Static nasal valve dysfunction is seen at rest, due to anatomic narrowness or obstruction; dynamic nasal valve dysfunction occurs when the patient inspires. Dynamic collapse is also described by the term lateral nasal wall insufficiency. The region of collapse can be divided into two zones, with Zone 1 roughly corresponding to the internal nasal valve and Zone 2 corresponding to the external nasal valve.2” (Position Statement: Nasal Valve Repair - American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS))
J34.82 Nasal valve collapse Instructional
J34.820 Internal nasal valve collapse
J34.8200 Internal nasal valve collapse, unspecified
Unacceptable Principal Dx (Inpatient Only)
J34.8201 Internal nasal valve collapse, static
Unacceptable Principal Dx (Inpatient Only)
J34.8202 Internal nasal valve collapse, dynamic
Unacceptable Principal Dx (Inpatient Only)
J34.821 External nasal valve collapse
J34.8210 External nasal valve collapse, unspecified
Unacceptable Principal Dx (Inpatient Only)
J34.8211 External nasal valve collapse, static
Unacceptable Principal Dx (Inpatient Only)
J34.8212 External nasal valve collapse, dynamic
Unacceptable Principal Dx (Inpatient Only)
J34.829 Nasal valve collapse, unspecified
Unacceptable Principal Dx (Inpatient Only)
Chapter 11 Diseases of the Digestive System
Anal fistula classification was updated at the March 8-9, 2022, Coordination and Maintenance Meeting. Anal fistulas and abscesses are the most common manifestations of perianal Crohn’s disease (CD). According to the ICD 10 Coordination and Maintenance Committee the existing ICD-10 codes did not distinguish between simple and complex anal fistulas and the required proxy codes to track the appropriate patient population. Despite differences in outcomes and treatment concepts, current ICD-10-CM Coding, K60.3 Anal Fistula, does not differentiate between simple versus complex fistulas, nor does it distinguish between unspecified, persistent, and recurrent fistulas. Creation of unique ICD-10-CM codes to differentiate between unspecified, persistent, and recurrent as well as simple vs. complex fistulas were created to advance patient care and long-term health outcomes through improved tracking and research.
There are 2 main classification systems referenced for fistulas, the American Gastrointestinal Society (AGA) and the Park’s classification. The anatomy of the rectum and anus is very distinct in drawing boundaries between the internal and external sphincters, and this is factored heavily in the Park’s classification.
Per the AGA they were noted in the lower tract, had a single opening, and no abscess, rectovaginal fistula, or anorectal stricture. Simple, fistulas were described in the treatment paradigm as non-IBD, intersphincteric and low transsphincteric fistulas involving less than 30% of the sphincter complex.
The AGA described complex fistulas as being located high-tract (high intersphincteric or high transsphincteric or extrasphincteric or suprasphincteric origin of the fistula tract) with multiple external openings, also with the presence of perianal abscess, rectovaginal fistula, or anorectal stricture, and these can be associated with the presence of active rectal disease on endoscopy. The treatment paradigm for complex fistulas described them as follows: “Complex Transsphincteric with >30% of external sphincter, suprasphincteric, extrasphincteric, horseshoe, and fistulas associated with IBD, radiation, malignancy, preexisting fecal incontinence, or chronic diarrhea.”
The full presentation can be found here Anal fistula.pdf The new codes are as follows:
K60.30 Anal fistula, unspecified
K60.31 Anal fistula, simple
Notes - Low intersphincteric anal fistula, Superficial anal fistula
K60.311 Anal fistula, simple, initial
K60.312 Anal fistula, simple, persistent
K60.313 Anal fistula, simple, recurrent
K60.319 Anal fistula, simple, unspecified
K60.32 Anal fistula, complex
Notes - Extrasphincteric anal fistula
High intersphincteric anal fistula
Suprasphincteric anal fistula
Transsphincteric anal fistula
Code also, if applicable:
perianal abscess (K61.0) (K61.0)
rectovaginal fistula (N82.3) (N82.3)
stenosis of anus and rectum (K62.4) (K62.4)
K60.321 Anal fistula, complex, initial
K60.322 Anal fistula, complex, persistent
K60.323 Anal fistula, complex, recurrent
K60.329 Anal fistula, complex, unspecified
K60.41 Rectal fistula, simple
Note - Fistula of rectum to skin
Code first, if applicable:
Crohn's disease (K50.-) (K50-K50.919)
ulcerative colitis (K51.-) (K51-K51.919)
congenital fistula (Q43.6) (Q43.6)
rectovaginal fistula (N82.3) (N82.3)
vesicorectal fistula (N32.1) (N32.1)
K60.411 Rectal fistula, simple, initial
K60.412 Rectal fistula, simple, persistent
K60.413 Rectal fistula, simple, recurrent
K60.419 Rectal fistula, simple, unspecified
K60.42 Rectal fistula, complex
Extrasphincteric rectal fistula
High intersphincteric rectal fistula
Suprasphincteric rectal fistula
Transsphincteric rectal fistula
Code also, if applicable:
perianal abscess (K61.0) (K61.0)
rectovaginal fistula (N82.3) (N82.3)
stenosis of anus and rectum (K62.4) (K62.4)
K60.421 Rectal fistula, complex, initial
K60.422 Rectal fistula, complex, persistent
K60.423 Rectal fistula, complex, recurrent
K60.429 Rectal fistula, complex, unspecified
K60.50 Anorectal fistula, unspecified
K60.51 Anorectal fistula, simple
K60.511 Anorectal fistula, simple, initial
K60.512 Anorectal fistula, simple, persistent
K60.513 Anorectal fistula, simple, recurrent
K60.519 Anorectal fistula, simple, unspecified
K60.52 Anorectal fistula, complex
K60.521 Anorectal fistula, complex, initial
K60.522 Anorectal fistula, complex, persistent
K60.523 Anorectal fistula, complex, recurrent
K60.529 Anorectal fistula, complex, unspecified
ELEVATE MEDICAL SOLUTIONS: YOUR TRUSTED PARTNER MEDICAL CODING
At Elevate, we’re dedicated to helping medical coders like you excel. Stay ahead of the curve by subscribing to our blog for the latest resources, industry insights, and exclusive webinars where you can earn AHIMA-approved CEUs—all for free.
Join Our Community Today!